Colorectal Cancer
About Colorectal Cancer
Colorectal cancers are the second most common cancer worldwide. It has always been a cancer of the western world. Traditionally, India had a lesser number of colorectal cancers but with urban India rapidly adopting a western lifestyle, the incidence is going up alarmingly. The lifetime chance of developing colorectal cancer is 1 in 22 for men and 1 in 24 for women.
Colorectal Cancer Risk Factors
- A personal or family history of colorectal cancer especially at a young age or polyps
- A diet with a lot of red and processed meats, low fiber, processed foods
- Inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis
- Conditions passed down through your families, such as familial
- Adenomatous polyposis (FAP)and hereditary nonpolyposis colon cancer (HNPCC)
- Obesity
- Smoking
Colorectal Cancer Symptoms
- A change in your bowel habits that doesn’t go away, such as constipation or diarrhea
- Blood on or in your stool
- Weight loss with no clear cause
- Unexplained Weakness or fatigue
- A lump in your abdomen or rectum
- A significant drop in Haemoglobin levels

Colorectal Cancer Diagnosis
Your doctor may give you a physical exam and feel your abdomen for any swollen organs or masses. They might also order one or more of these tests to spot polyps or colorectal cancer :
- Rectal exam. Your doctor can use their fingers to feel for growths in the rectum
- Colonoscopy. This is the standard screening test that experts recommend. Your doctor uses a thin, flexible tube called a colonoscope to look at your entire colon and rectum.
- Biopsy. During a colonoscopy, your doctor may take out a bit of tissue and send it to a lab for testing. This helps identify the type of tumor and plan the treatment ahead. Complications are rare, but you may have some bleeding or discomfort
- CT scan/ PET scan. these are commonly done tests to look at the extent of spread and get an idea about the stage of cancer.
- MRI is more commonly used in rectal cancers for accurate assessment of spread and deciding on the further course of treatment.
Treatment Options

Surgery
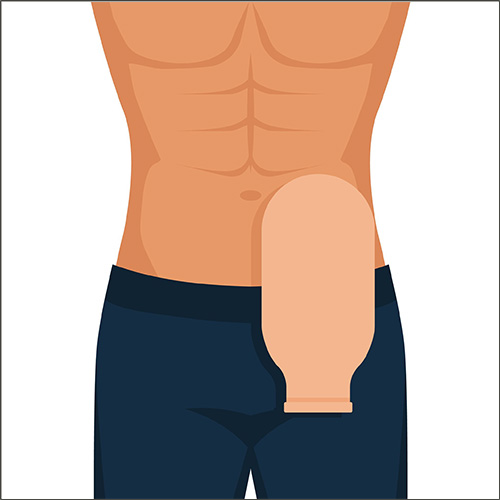
Surgery is the most common initial treatment for colorectal cancer. During surgery, the tumor, a margin of the surrounding healthy intestine, and adjacent lymph nodes are removed. In patients with rectal cancer, the affected part of the rectum with a good margin is removed and the remaining ends are joined by means of a stapler. The rectum sometimes is permanently removed if cancer arises too low in the rectum. The surgeon then creates an opening (colostomy) on the abdominal wall through which solid waste from the colon is excreted. Specially trained nurses (Enterostomal therapists) can help patients adjust to colostomies, and most patients with colostomies return to a normal lifestyle. Surgery can be either minimally invasive in the form ofRobotic/ Laparoscopic or Open surgery. Evidence has shown that there is rapid recovery, less pain, and an early return to work when it is performed with a minimally invasive approach. However, it has to be selected appropriately as per the patient type/ location, and stage of cancer.
Radiation Therapy
This modality is usually used in rectal cancers to reduce the size prior to surgery. nowadays, highly precise radiation techniques are available like IMRT and IGRTto target the tumor and reduce effects on the surrounding tissues. In rectal cancers, radiation is either short course or long course. This modality has changed the outcomes for rectal cancers amazingly and many patients with low rectal cancers now are spared a permanent colostomy due to the shrinking of these tumors prior to surgery by radiation. Pre-operative radiation has also improved long-term survival in rectal cancers.
Chemotherapy
Chemotherapy drugs destroy cancer cells at a cellular level and stop them from spreading. While many of these drugs are intravenous, some are also available in oral form. Some work better together, so you may take two or more at the same time. Usually, this is given as a combination of multiple drugs in the form of cycles at 2 or 3 weekly intervals You might have chemotherapy after surgery or you could have it before surgery to make the cancerous tumor smaller and easier to remove.
Colorectal Cancer Prevention
- Healthy tobacco-free lifestyle
- Exercise and a healthy lifestyle (The American Cancer Society says adults should get 150 minutes of moderate-intensity or 75 minutes of high-intensity exercise (or a combination of these) each week.
- a low-fat, high-fiber diet that includes at least 2 1/2 cups of fruits and vegetables each day
- Cut back on red meat and other high-fat foods
- Avoid overcooking or barbecuing meats and fish.
- Screening for colorectal cancer
- Genetic counseling and testing
Surgery for Colon and rectal cancers
Surgery is often the main treatment for early-stage colon cancers. The type of surgery used depends on thestage(extent) of cancer, where it is in the colon, and the goal of the surgery.
Any type of colon surgery needs to be done on a clean and prepared colon. The patient may be advised aspecial diet before surgery and may need to use laxative drinks and/or enemas to get all of the stool out of the colon..
Colectomy
A colectomy is a surgery to remove all or part of the colon. All the lymph nodes which drain the affected area are also removed. This is called a radical colectomy.
- If only part of the colon is removed, it’s called a hemicolectomy, partial colectomy, or segmental resection.
- The remaining sections of the colon are then reattached. This is usually done by means of a surgical stapler.
If the entire colon is removed, it’s called a total colectomy.
A colectomy can be done in 2 ways:
- Open colectomy: The surgery is done through a single long incision (cut) in the abdomen (belly).
- Laparoscopic-assisted or robotic-assisted colectomy: The surgery is done through smaller incisions and special tools. Because the incisions are smaller in a laparoscopic-assisted or robotic colectomy than in an open colectomy, patients often recover faster and may be able to leave the hospital sooner than they would after an open colectomy… We routinely perform laparoscopic and robotic colectomies. However, it may not be the best approach for large or bulky tumors. it is important to remember that the main aim has to be complete and radical removal of the tumor safely rather than avoiding a scar.

Rectal cancer
Surgery is usually the main treatment for rectal cancer. Radiation and chemotherapy are often given before the surgery.
Transanal excision (TAE)
This surgery can be used to remove some early-stage I rectal cancers that are relatively small and not too far from the anus.
Low anterior resection (LAR)
Some rectal cancers in the upper or mid part of the rectum can be removed by low anterior resection (LAR). In this operation, the part of the rectum containing the tumor is removed along with the draining lymph nodes The rejoining of the colon with the rectum is done by means of a stapled device.
Sometimes, a temporary stoma is given to divert the stool, and that allows the joint to heal well. This stoma is reversed later by a surgical procedure.
Abdominoperineal resection (APR)
This operation is needed if the cancer is growing into the sphincter muscle (the muscle that keeps the anus closed and prevents stool leakage)
Here, the anus is removed along with the rectum, and a permanent colostomy is needed (the end of the colon is connected to a hole in the skin over the abdomen) to allow stool to pass.
All types of surgeries for rectal cancers can be performed by either laparoscopic, robotic, or open approaches depending on various factors.
Follow-up tests
What types of screenings you have and how often you get them will depend on the type and stage of cancer you had and the treatments you got. You’ll probably need check-ups three to four times a year during the first 2 or 3 years after treatment and one or two times a year after that. These might include:
- A physical exam
- Colonoscopy, usually 6 months to 1 year after surgery. Your doctor can tell you how often you’ll need one.
- CT scans of your chest, abdomen, and possibly pelvis every 6 to 12 months for the first 3 years
- CEA (carcinoembryonic antigen) blood test every 3 to 6 months for 5 years. High levels of CEA protein in the blood may mean cancer cells have spread.
Colorectal Cancer Prevention
- Healthy tobacco-free lifestyle
- Exercise and healthy lifestyle (The American Cancer Society says adults should get 150 minutes of moderate-intensity or 75 minutes of high-intensity exercise (or a combination of these) each week.
- A low-fat, high-fiber diet that includes at least 2 1/2 cups of fruits and vegetables each day
- Cut back on red meat and other high-fat foods
- Avoid overcooking or barbecuing meats and fish.
- Screening for colorectal cancer
- Genetic counseling and testing
Book an Appointment
Related Blogs
Why are my Stools Black ? Key reasons and what to do?
If you’ve recently noticed that your stools have turned black, it’s natural to wonder if it’s a cause for concern. In India, where digestive…
Causes and Symptoms of Liver Cancer
Liver cancer is one of the fastest-growing cancers worldwide, with a high prevalence in countries like India due to risk factors such as hepatitis...
Top Treatment Options for Esophageal Cancer with Dr Ganesh Nagarajan
Esophageal cancer is a serious condition requiring highly specialized care, as it affects the esophagus—a critical part of our…
Related FAQ’s
1. Can I lead a normal life after surgery for colon cancer?
Yes, you will lead an absolutely normal life after this surgery. Many survivors get back to work in a few weeks, socialize and play sports, swim, and live fulfilling lives after their treatment.
2. If I have a stoma, how do I live with it?
A stoma may be temporary or permanent. Usually, your doctor and/or stoma nurse will help you learn how to manage the stoma bag. There are support groups to help you cope with the issues you may face. People lead normal lives once they get used to having a stoma.
3. After a rectal cancer surgery, what complications can I expect?
These are usually very safe surgeries and more than 95% of patients sail through the operation. Some patients may have issues like bleeding, infection, leakage from the joint site, or clots in the legs. Many of these are treatable while a small percentage may be potentially life-threatening.
4. Can these surgeries affect sexual functions?
Most patients will have normal sexual functions after colorectal surgeries. A few men after a low rectal cancer surgery may face some dysfunction that may need medical assistance.
5. Can I have a normal diet after colorectal surgery?
Yes. You can return to a normal diet once you have recovered from your surgery. It would be advisable to have a high-fiber and low-fat diet in moderation and avoid constipation.
6. Is colorectal cancer hereditary?
In some cases, it is but in most cases it isn’t. There are various genetic tests especially advised in young patients with colorectal cancer or those with multiple cancers or cancer in the background of multiple polyps. A genetic counselor may advise tests for the other family members in some such scenarios.